About Angelman Syndrome
AS Genotypes: UPD
Uniparental disomy (UPD) is when both copies of a chromosome pair came from one parent, instead of the usual one chromosome from the egg, one chromosome from the sperm. UPD AS happens when both copies of chromosome 15 came from the father. Because the paternal UBE3A gene is always turned off in neurons, when both copies of chromosome 15 come from the father, both UBE3A genes are turned off, and no UBE3A protein is made in the brain.
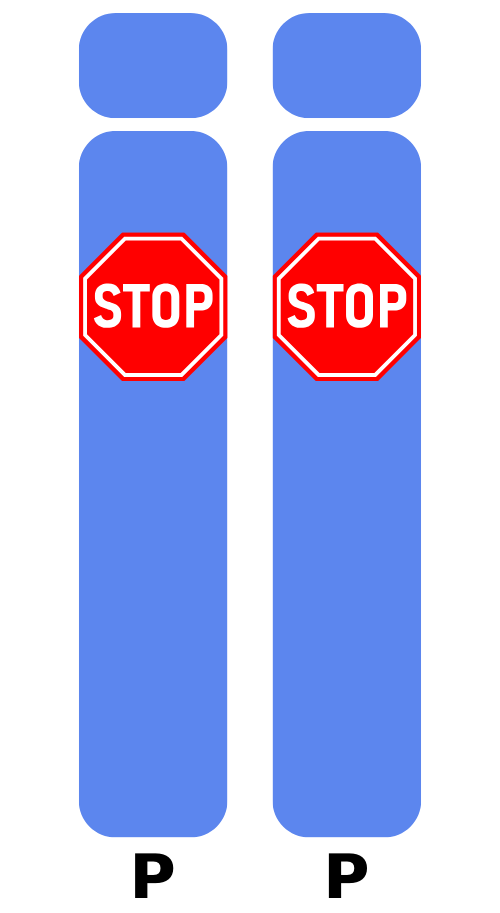
There are two different types of UPD, called heterodisomy (the two chromosomes from the sperm are different from each other) and isodisomy (the two chromosomes from the sperm are exactly the same). The type of UPD does not affect which symptoms or characteristics of AS an individual has. However, it can affect the ability to get diagnosed, since some tests can only detect isodisomy. Learn more about genetic testing for AS at Testing 101.

In most cases, UPD is a random event that occurred in the formation of the sperm or egg, or early in the development of an embryo. However, sometimes UPD is the result of a chromosome difference in a parent that makes UPD more likely to occur. Consequently, chromosomal testing of the parents is recommended. If the parents have chromosomal testing that is typical, the chance for a future child to have UPD that causes AS is predicted to be less than 1%. This means that at least 99% of the time, future children will not have UPD that causes AS. This chance is not zero because rare cases have been reported where chromosome 15 is more likely to be packaged incorrectly when eggs are made, resulting in an increased chance for UPD. If a parent has a chromosomal difference, the chance will depend on the specific chromosomal difference.

How is UPD AS different from other AS genotypes?
UPD is functionally similar to ICD, so you may see them grouped together in the AS literature. In contrast to Deletion AS, where multiple genes on the maternal chromosome 15 are missing, those living with UPD are not missing a single piece of DNA—which generally makes their features less severe.
Like UBE3A is only turned on from the maternal chromosome 15, there are other genes in that region of chromosome 15 that are only turned on from the paternal chromosome 15. Individuals with UPD are making extra of the proteins from those genes that are turned on the paternal copy of chromosome 15.

In general, having missing genes and proteins (like missing UBE3A!) causes more symptoms than having extra copies of genes and making extra proteins. The vast majority of the symptoms an individual living with UPD AS experiences are because of the absence of UBE3A. However, making extra of these paternally expressed proteins (over-expression) may explain characteristics that have been described in some individuals living with UPD AS, including increased appetite and risk for obesity.
FAST puts enormous resources behind fighting for the inclusion of UPD/ICD in both research as well as clinical trials. All the pharma companies in our space have stated that they want to have the most consistent group for the earliest phases of clinical trials (Phase 1/2), and in many cases they want the most severely affected to start with. That is generally considered deletions. Once they can show safety (Phase 1) and early efficacy (Phase 2)—which are generally run together in trials as a Phase 1/2—then they will likely add a cohort of other genotypes.
You can read more about the future of UPD/ICD inclusion in trials in this Q&A with FAST Chief Science Officer Allyson Berent.
Connect with other AS UPD families by writing to us here: community@cureangelman.org
Still have questions?
If you are wondering about your specific chance to have a child with a genetic variant that causes AS, it is very important to consult a genetics professional like a genetic counselor or geneticist. The chance varies depending upon the test results of the person living with AS and the testing that was performed on the parent(s). The information provided here may be helpful but it is not specific to your family and is not meant to replace genetic counseling.